
Featured
Overview
LupusCorner
Symptoms
LupusCorner
Diagnosis & Tests
LupusCorner
Living With Lupus
LupusCorner
Resources
LupusCorner

The LupusCorner Toolkit
Stay up-to-date on research. Use apps designed to support life with lupus. Get access to a community of people that understand the challenges you are going through.
Check out these other LupusCorner tools:












































































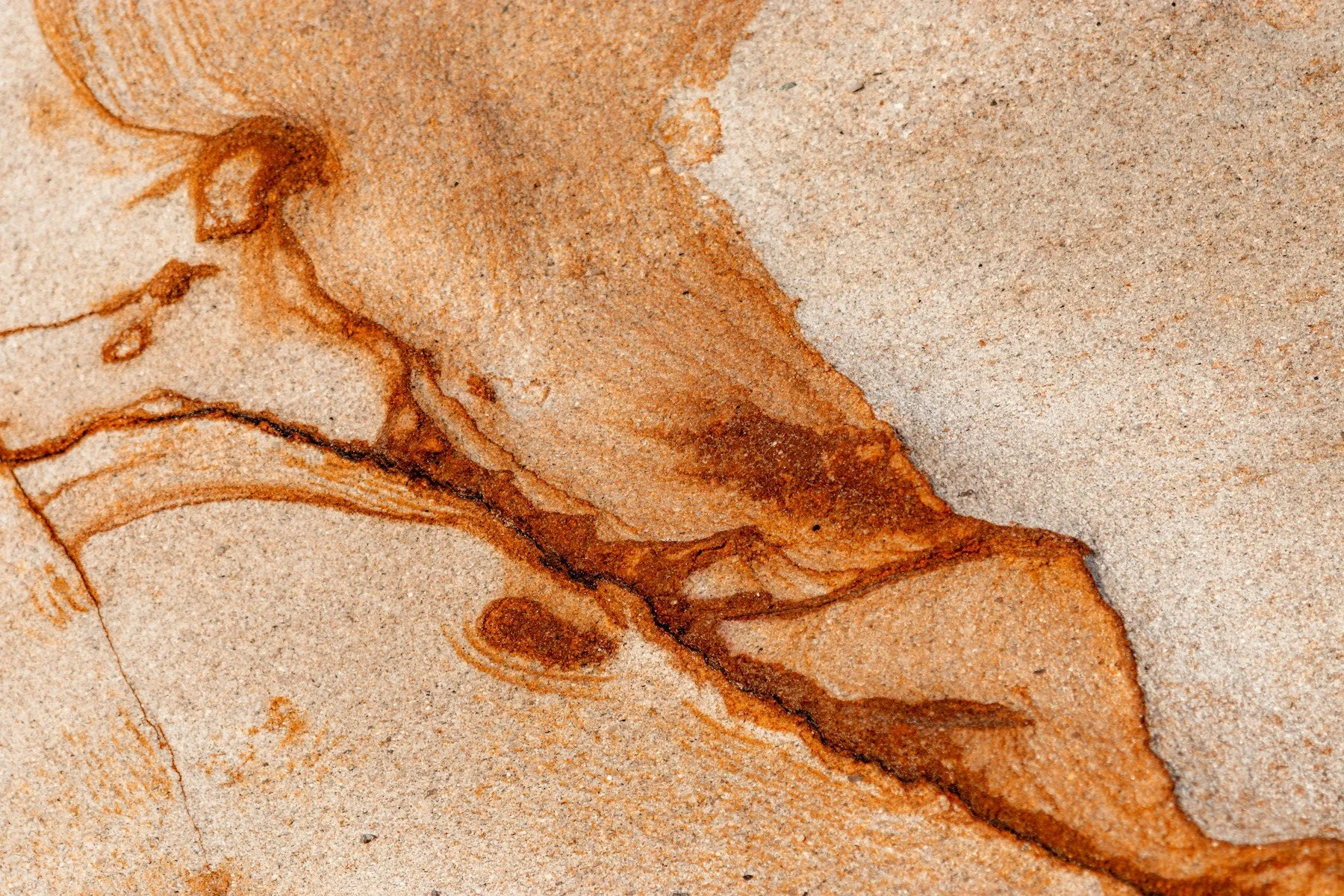





























Vasculitis affects nearly half of people with lupus and occurs when inflammation targets the blood vessels, restricting blood flow and causing symptoms that can appear anywhere in the body. Understanding how vasculitis develops, what signs to watch for, and why it matters can help you recognize changes earlier and advocate for the right care.