
Featured
Overview
LupusCorner
Symptoms
LupusCorner
Diagnosis & Tests
LupusCorner
Living With Lupus
LupusCorner
Resources
LupusCorner

The LupusCorner Toolkit
Stay up-to-date on research. Use apps designed to support life with lupus. Get access to a community of people that understand the challenges you are going through.
Check out these other LupusCorner tools:












































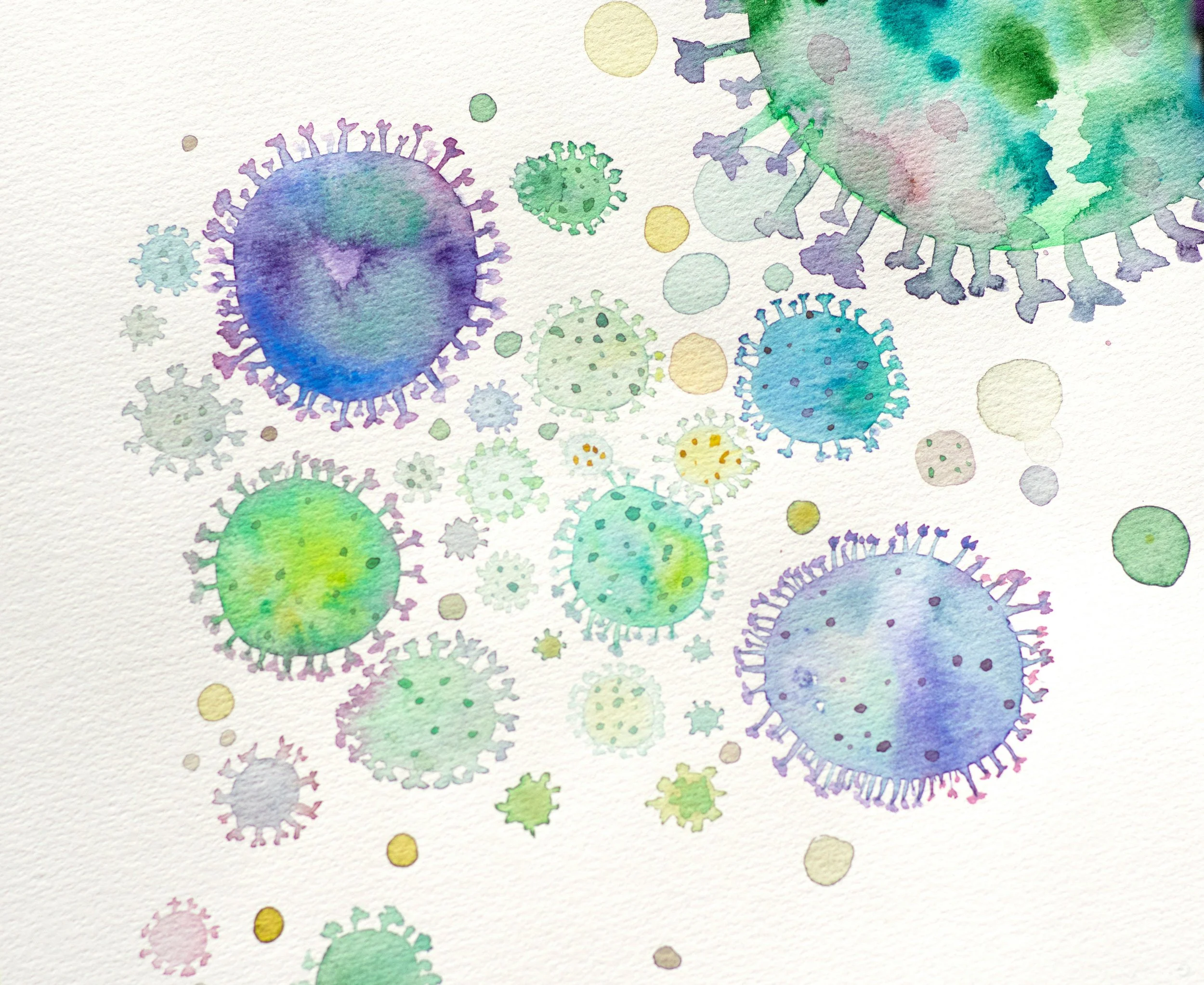





























































For people living with lupus, thyroid problems are more common — and their symptoms can overlap with lupus flares, making them difficult to spot. Fatigue, weight changes, sensitivity to hot or cold, and mood changes could all point to thyroid imbalance. Understanding how lupus affects the thyroid can help you recognize symptoms early and ask your doctor about testing.